Winter might be cozy, but if your fingers or toes turn white, blue, or red with the cold or stress, it could be more than just the chill.
You might be experiencing Raynaud’s Syndrome — a condition that causes blood vessel narrowing and reduced blood flow to extremities, potentially leading to long-term damage if left unmanaged.
Let’s explore the symptoms, how to diagnose it with a Raynaud’s Syndrome [1] test, ways to get relief naturally, and what to do during an unexpected attack.
What Is Raynaud’s Syndrome?

Raynaud’s Syndrome — also known as Raynaud’s Disease or Raynaud’s Phenomenon — is a condition where small blood vessels constrict excessively in response to cold or emotional stress.
This leads to reduced blood flow, most commonly in the fingers and toes, but it can also affect the nose, ears, lips, and even nipples.
This exaggerated response, caused by vasospasm of small blood vessels due to an overactive sympathetic nervous system, leads to cold, numb, and discolored extremities, typically white or blue, due to oxygen-deprived blood pooling in narrowed vessels.
Once normal blood flow returns, the skin may flush red, tingle, or throb.
There Are Two Types of Raynaud’s
- Primary Raynaud Phenomenon: Occurs without any underlying condition. It’s usually milder and more common.
- Secondary Raynaud Phenomenon: Associated with autoimmune disorders or connective tissue diseases like rheumatoid arthritis, lupus, or scleroderma. This form tends to be more severe and may cause lasting damage, such as ulcers or tissue death.
What Triggers Raynaud’s Attacks?
Triggers that may provoke an episode include:
- Cold weather
- Holding a cold drink or touching frozen items
- Emotional stress or anxiety
- Air conditioning
- Sudden temperature changes
These can all trigger blood vessel narrowing, making the skin in affected areas turn pale or blue, followed by numbness or pain.
Raynaud’s Syndrome Test and Diagnosis

Wondering if you have Raynaud’s? A proper diagnosis includes:
- Medical History & Physical Exam: Your healthcare professional will assess your symptoms and ask about patterns related to cold or stress.
- Cold Stimulation Test: Although less commonly used today due to discomfort, this test involves immersing fingers in cold water to evaluate delayed blood flow recovery, potentially indicating Raynaud’s Syndrome. Delays may indicate Raynaud’s Syndrome.
- Nailfold Capillaroscopy: A drop of oil is placed at the base of the fingernail and examined under a microscope. Enlarged or damaged capillaries often suggest secondary Raynaud’s.
- Blood Tests: To check for autoimmune disorders, including the antinuclear antibody (ANA) test and thyroid stimulating hormone (TSH) levels.
Dr. John Gorski, a hand and wrist specialist at Michigan Surgery Specialists, emphasizes the importance of a comprehensive evaluation when diagnosing Raynaud’s syndrome. He notes that while there is no single definitive test for Raynaud’s, a combination of patient history, physical examination, and specific diagnostic procedures can effectively distinguish between primary and secondary forms of the condition.
Common Risk Factors
Raynaud’s can affect anyone, but the risk increases if you:
- Are female (especially of childbearing age)
- Have a family history
- Suffer from autoimmune diseases or skin diseases
- Use vibrating tools regularly
- Smoke cigarettes
- Have had chemotherapy or injuries to the hands
- Take medications for high blood pressure, ADHD, migraines, or decongestants. Certain medications, including beta-blockers, chemotherapy agents, and migraine drugs (like ergotamine), may induce or worsen symptoms
Symptoms of Raynaud’s Syndrome
- Cold hands and feet that feel cold even indoors
- Color changes: white, then blue, then red upon warming
- Numbness, tingling, or stinging pain in affected areas
- Severity and frequency of symptoms can vary widely among individuals, with secondary Raynaud’s generally presenting more severe complications
- In severe cases: skin ulcers or tissue damage
What to Do During a Raynaud’s Attack
Caught up in a flare-up? Here’s what to do right away:
- Get Warm Fast: Move to a warmer space if possible.
- Use Body Heat: Tuck fingers into your armpits or sit on your hands to warm them naturally.
- Gentle Movement: Wiggle your fingers and toes to stimulate blood flow.
- Soak in Warm Water: Immerse your hands or feet in warm (not hot) water to encourage circulation.
- Stay Calm: Emotional stress can worsen symptoms, so practice deep breathing to relax.
Home Remedies to Improve Blood Flow
These lifestyle strategies can make a big difference:
1. Layer Up Year-Round

Invest with thermal gloves, heavy socks, insulated boots, and layered clothing. Keep your core warm – even indoors – to help maintain extremity circulation.
2. Exercise Regularly

Physical activity supports healthy blood flow and helps prevent blood vessel narrowing. Aim for low-impact heart-healthy routines, and always stay warm during workouts.
3. Stress Management

Deep breathing, meditation, yoga, or even hobbies like crafting or coloring can lower emotional stress and reduce flare-ups.
4. Acupuncture
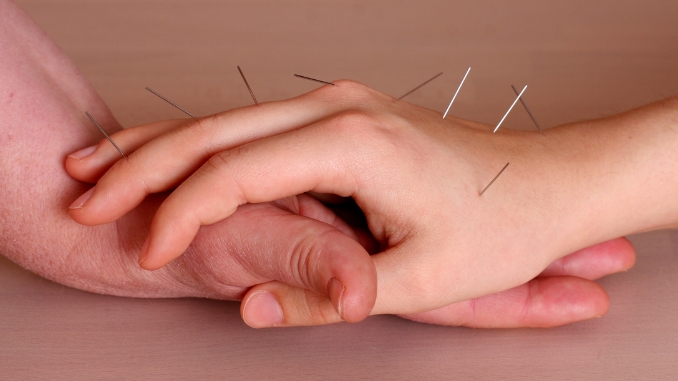
Preliminary studies suggest acupuncture [2] may improve circulation and reduce the frequency of Raynaud’s attacks, especially in primary Raynaud patients. Although more robust research is needed.
5. Ginkgo Biloba

This natural supplement may support circulation and reduce attack frequency. One study showed a 56% reduction in attacks with regular use.
6. Fish Oil

Omega-3 fatty acids can help reduce sensitivity to cold and may improve circulation. Choose high-quality fish oil supplements [3] with a daily dose approved by your healthcare provider.
7. Stop Smoking, Caffeine & Alcohol
Smoking cigarettes can cause the blood vessels in your body to constrict and damage them as well. If you smoke, do your best to quit.
8. Avoid Your Triggers
Whether your symptoms arise because of cold temperatures, stress, or emotional upset, your best approach is to try to avoid these triggers. Stay warm and practice daily stress relief and mindfulness to keep your emotions even and centered.
9. Treat an Attack Immediately
If you notice the condition flaring up, don’t wait — take immediate action. The best approach is to get to a warm location and soak your hands and feet in warm, not hot, water. If this isn’t possible, wiggle your fingers and toes and try to get them somewhere else warm. You may put your fingers under your armpits, for example, or massage your feet.
10. Avoid Alcohol

It’s important to avoid alcohol because it can interfere with blood circulation. Alcohol may cause blood vessels to constrict or dilate unpredictably, which can trigger or worsen Raynaud’s attacks—leading to cold, numb, or discolored fingers and toes. Staying away from alcohol helps maintain stable blood flow and reduces the risk of flare-ups.
When to See a Doctor
If your symptoms are frequent, severe, or worsening — especially if you notice sores, skin ulcers, or signs of tissue damage — consult your healthcare provider. You may need calcium channel blockers or other medications to improve blood flow and prevent complications.
Raynaud’s can be linked to serious underlying diseases such as:
- Rheumatoid arthritis
- Scleroderma
- Lupus
- Polymyositis
- Thyroid disorders
- Other autoimmune diseases
Early diagnosis can help prevent permanent damage to affected areas.
Final Thoughts
Raynaud’s Syndrome is often manageable with lifestyle changes and awareness. Knowing your triggers, learning how to react during an attack, and speaking to your doctor about the right Raynaud’s Syndrome test can go a long way in improving your quality of life.
Don’t ignore those cold hands — your fingers (and toes) will thank you!
You can use the coldest part of the year to improve your health in multiple ways. Check out this Winter Wellness Bundle now!
Frequently Asked Questions
What is the difference between primary and secondary Raynaud’s Syndrome?
Primary Raynaud’s occurs without any other associated health conditions and is generally mild. Secondary Raynaud’s, also known as Raynaud’s phenomenon, is linked to autoimmune or connective tissue diseases like lupus or scleroderma and can lead to serious complications, including skin ulcers and tissue death.
Can Raynaud’s be permanently cured?
There is no known cure for Raynaud’s Syndrome. However, symptoms can often be managed effectively with lifestyle changes, medications like calcium channel blockers, and avoiding triggers that cause blood vessel narrowing.
What kind of doctor should I see for Raynaud’s Syndrome?
Start with a family physician or general practitioner. If secondary Raynaud’s is suspected, you may be referred to a specialist, like a rheumatologist, who focuses on autoimmune and musculoskeletal diseases.
How is Raynaud’s disease diagnosed?
Diagnosis typically includes a physical exam, a review of your medical history, and various diagnostic tests such as a Raynaud’s Syndrome test (cold stimulation), nailfold capillaroscopy, and blood tests for autoimmune markers like the antinuclear antibody (ANA) or thyroid-stimulating hormone (TSH).

Rick Kaselj MS, is a leading kinesiologist and injury specialist as well as co-creator of the best-selling Unlock Your Hip Flexors program. Rick creates exercise programs that help people heal injuries and eliminate pain, so they can go back to living a full, active, healthy life.



